
Improve Care with Informed Decisions and Efficient Reviews
Claim Clarity helps utilization review professionals focus on what they do best: Provide safe, sound, and effective treatment determinations for improved patient outcomes.
Contact for a consultationInstant Authorization and UR Triage with All Guidelines in a Single Place
Save time and effort for a hyper-efficient process to identify the appropriate and safe treatment for every review. Claim Clarity consolidates all state and evidence-based guidelines in a unified repository. All guidelines are automatically updated, in real-time, to equip reviewers with the latest information, for the most accurate and effective decisions.
The fully automated solution provides instant authorization of claims if recommended care is consistent with state or evidence-based guidelines. The system identifies those circumstances with exceptions to guidelines and reroutes them for formal utilization review.

Map Unstructured Data for Accurate Decisions
Accurately define injuries to determine the most appropriate treatment outcomes by mapping free-form patient data into standardized ICD and CPT codes. Simply enter the nature of the injury or recommended treatment in your own words. Claim Clarity will instantly align the descriptions in free-form text with standardized codes through semantic modeling.
Developed by medical professionals with industry and domain expertise, Claim Clarity streamlines unstructured patient data, refined to the distinctive requirements of workers’ compensation insurance. The solution is deigned to give users the confidence to make informed decisions for accurate treatment outcomes.
Learn more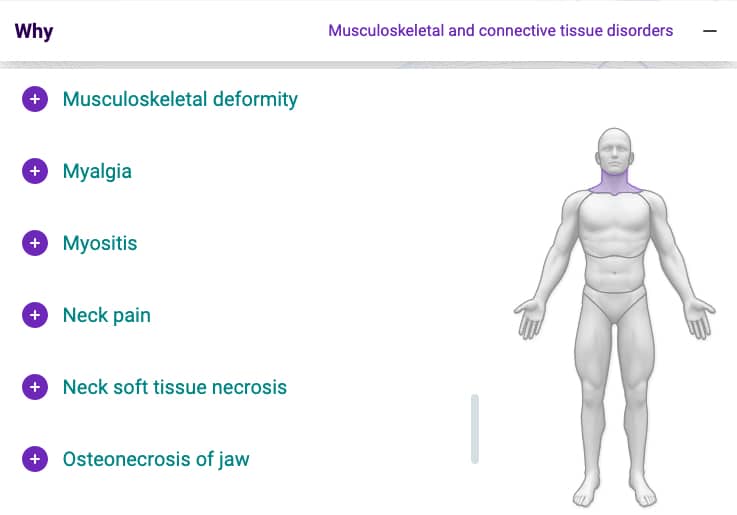
AI Assistant for Improved Utilization Management Performance
Claim Clarity is built on an artificial intelligence engine that learns from millions of historical workers’ compensation claims. AI leverages this clinical intelligence to provide authorization recommendations, and offer care guidance. Smart, dynamic algorithms assist you in determining if care is consistent with guidelines, detects those circumstances where recommended care deviates from guidelines, and diverts those requests that require human intervention to peer review.
AI is the decision support tool that gives UR professionals the confidence to make well-informed decisions that deliver high-quality care to return employees back to work safely.
Learn more
Claim Clarity is a Trusted Partner of ODG

Improve Peer-to-Peer Collaboration
A unified source of standardized, AI-powered data helps providers determine the most effective care consistently, for every claim. Claim Clarity improves process efficiency and collaboration for all stakeholders at any stage during the course of treatment, from pre-authorization to concurrent and retrospective reviews, and appeals. The solution facilitates submission and processing of requests for timely rendering of UR and peer review decisions, and prevents unnecessary delays in patient care.
Build a Solid Rationale with Findings
Claim Clarity provides support for medical necessity determination by outlining relevant findings with sound reasoning and defensible rationale. Turning precedent case and utilization data into actionable predictive insights, the solution helps UR professionals build confidence in their decisions that improve patients’ well-being.