
Let AI Do the Work for Better Outcomes in Record Time
A decision support solution for claims adjusters, case managers, review nurses, and healthcare providers across the workers’ compensation ecosystem.
Contact UsInstant Access to All Guidelines
Access the right guideline by simply selecting the state where the incident occurred on a map. If the state uses evidence-based guidelines, the system will automatically search those guidelines, updated in real time. The solution reviews all available evidence-based practice guidelines, from a single repository. It confirms compensability through real-time authorization to save time for claims adjusters, case managers, nurses, and everyone who touches a workers compensation claim. Most importantly, patients receive the critical care they need without delay.

Standardized Search for All Conditions and Procedures
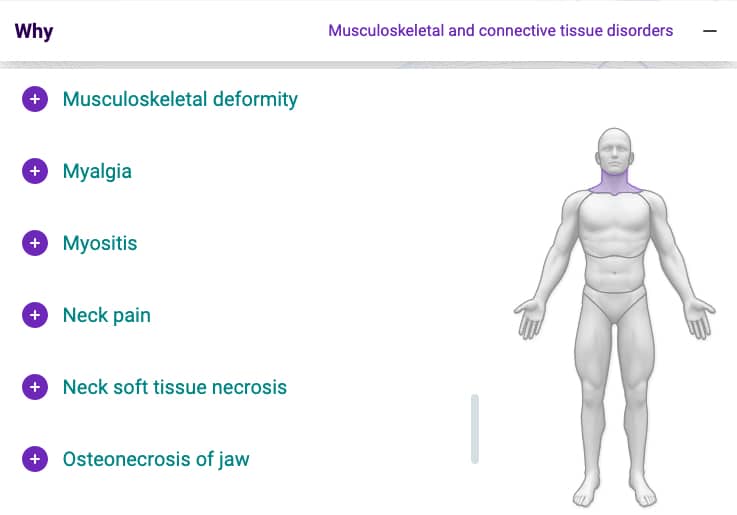
Defining the condition with precision and finding the right treatment is easier than ever with a solution that supports your team no matter how fluent they are in medical terminology. You can now simplify your reviews with an easy search by condition, procedure, medical code, or body part, in an intuitive application developed exclusively for workers’ compensation professionals.
Claim Clarity has mapped all possible conditions to correlating treatments through semantic modeling. You can simply describe the condition in your own words, which AI will automatically map into standardized terminology for authorization. Or, if known, you can enter the ICD or CPT code, which the system will instantly align for efficient claim management. Better yet, you can select the body part to pinpoint the exact location of the injury from an anatomical diagram, saving you time, and improving the accuracy of your claims.
Furthermore, your teams can quickly identify if the treatment requires a formal review for medical necessity. If it does, they can easily retrieve the relevant treatment guideline based on the jurisdictional requirements of the benefit state, then apply the treatment criteria, and finally create a formal determination which can be sent back to the requesting care provider with detailed rationale explaining what criteria was used to support medical necessity for the treatment requested.
Instant authorization with AI
Claim Clarity’s AI engine processes millions of historical workers’ compensation claims to help you make informed decisions. Reviewing precedent, AI clinical intelligence can provide authorization recommendations, and offer care guidance with an extra layer of verification. For those rare incidents that deviate from guidelines or that don’t have a historic precedent for treatment, the system will reroute them to a clinical review. This rigorous process saves time and the cost of unnecessary utilization reviews, while ensuring that all appropriate options are exhausted to authorize or approve a treatment.

Data analytics for actionable Insights
Claim Clarity’s powerful AI offers the opportunity for providers, administrators, government and legal organizations to transform their data into actionable insights. Smart, dynamic algorithms learn from every case to predict outcomes for future cases. The technology is trained to provide a view into how a claim will likely resolve, based on the initial input parameters. Predictive analytics help your teams assess the risk for short term and long term disability scenarios and durations, make optimized reserve decisions, adjust staffing levels, and take action to shorten return to work timelines. Prescriptive recommendations equip your organization with the strategic capabilities that it needs to improve patient outcomes, lower costs, reduce administrative and RTW timelines and improve profitability.

The Latest Technology for the Essential Truth
Leverage Claim Clarity’s powerful AI to improve claim outcomes, save time and reduce costs instantly
Seamless Integration with a Simple API
You can access Claim Clarity directly on the web through an application with an intuitive interface. You can also integrate it to your existing system with a simple API for a seamless experience. You can connect to the solution for end-to-end claim and utilization management, or choose the module you need to tailor the experience for your unique business needs.
Confidence in the Cloud
Our cloud-based application updates data in real time, allowing your distributed users to access the most accurate insights from anywhere, any time. Fast and fluid processing with breakthrough performance and continuous availability provide a smooth and efficient solution with no downtime.
Secure in the Knowledge
Claim Clarity is built on a security-first cloud architecture. Centralized data backups lower the risk of data loss and allow for disaster recovery. The solution uses data encryption to ensure data privacy, and compliance with HIPAA guidelines, protecting your organization’s security mandate.